Original author: Dr Jasmeen Sethi
Original published date: 21st April 2014
Article updated by: Dr Hafsa Waseela Abbas
Updated article date: April 2025
Review date: April 2027
About
Dr Jasmeen Kaur Sethi is the Assistant Product Manager at Roche. She was amongst the initial supporters of the FST where she encouraged and wrote a one-off article voluntarily about cancer.

According to the latest reports by the World Health Organisation (2025), cancer is the leading global cause of death and there were approximately ten million deaths in 2020. The mortality rate is decreased if cancer is both detected and treated early. It is estimated that almost half of cancer cases in the UK are late-stage staged and screening programs are limited to cervical, breast, colon, and lung (National Institute for Health and Care Research (2025). Early detection has two components: techniques to diagnose early and screening programs to increase survival rates and improve the quality of life.
The World Health Organisation and its partnerships as part of the 2030 UN Agenda for Sustainable Development, aim to commit to research to understand the risk factors, causes, and pathogenesis of cancer. To identify, develop, and monitor cost-effective strategic tools and standards for early diagnosis, screening, cancer prevention, and palliative care for adult and childhood cancers. Health promotion, technical assistance, timely diagnosis, and access to care are among the objectives. The role of policymakers and regional networks is fundamental to strengthening the healthcare systems on a local and national level to improve accessibility to cancer treatments and screening. Key examples are the Global Strategy to Accelerate the Elimination of Cervical Cancer, the WHO Global Initiative for Childhood Cancer, and the Global Platform for Access to Childhood Cancer Medicines (World Health Organisation, 2025).
Symptoms
Awareness of the signs and symptoms of different cancers is necessary to find the cause. During the consultation with the healthcare professional, a discussion of the clinical history, duration, and severity score of the symptoms, feelings, and concerns. Careful questioning, listening, and understanding of verbal and non-verbal communication conducted by the patient is necessary. An empathetic attitude is applied regularly to build rapport in patient-doctor communication. This helps to develop a factual account yielding a provisional diagnosis of the patient’s illness and determine the relevant investigations (Innes, 2009).
Symptoms of cancer are dependent on the type of tumour, however, general signs and symptoms in suspected cancer cases are in Figure 1 (Cancer Research UK, 2022). Feeling more tired than usual, pain around the body, and more noticeable weight loss for no defined reason can signify cancer and may require further investigations. Blood in the urine or stools, feeling sick (nausea), or vomiting are common symptoms of cancer. Sweating and high temperature may indicate fever, infections, and night sweats. However, these symptoms may overlap with menopause. Similarly, bleeding (red, brown, or black) discharged from the vagina pre, during, or post-sexual intercourse may also signify menopause. In addition, Lumps and swelling particularly in the lymph nodes in the neck, armpit, chest, breast, stomach, or testicle require further examination (Cancer Research UK, 2022).
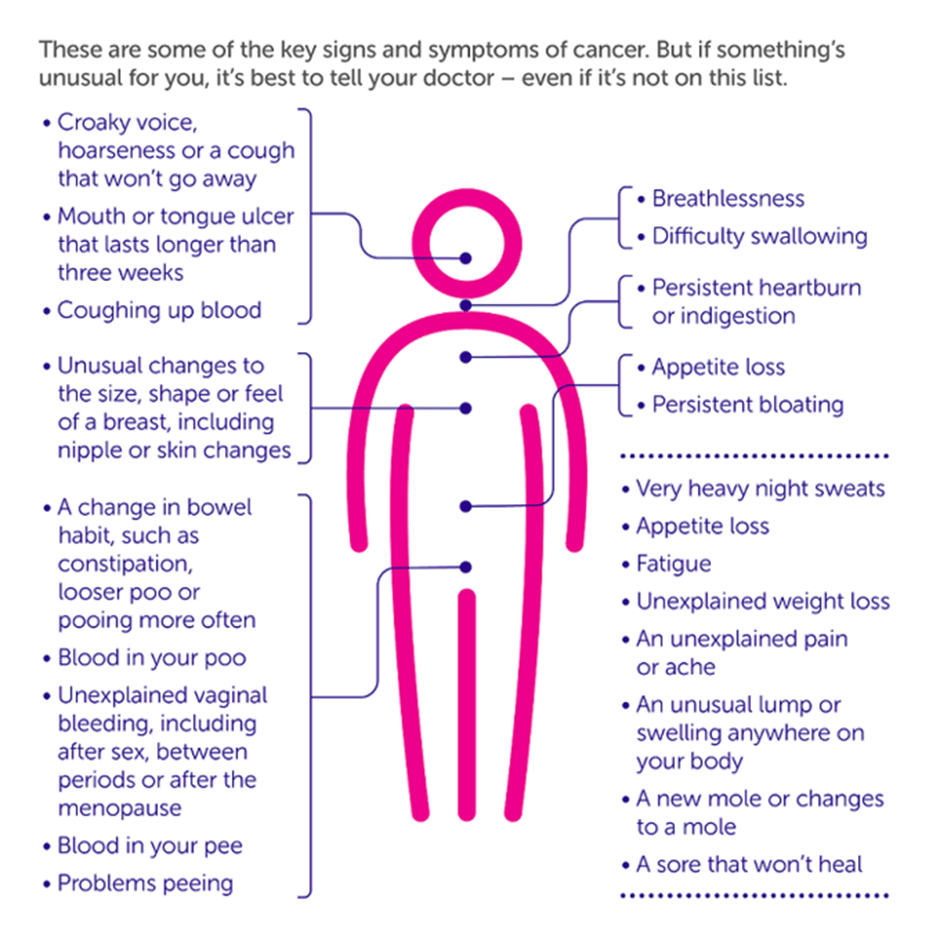
Figure 1: Some of the most common signs and symptoms in every cancer (Cancer Research UK, 2022)
Physical Examination
This step is necessary to explore the symptoms the patient is experiencing and maintaining the dignity of the patient is essential. The patient must feel comfortable, and aware of what the procedure involves and may include a chaperone (Innes, 2009). For instance, in suspected cases of breast cancer, medical attention is paid to the lump and tender areas which may give a sense of anxiety, timidness, or embarrassment.
Upon establishing the site and pain (mastalgia), the healthcare professional may determine the following as part of his or her examination (Thomas and Monaghan, 2007).
- Pain is unilateral (one breast) or bilateral (two breast)?
- Heat or redness in the area?
- A colour change of the skin?
- Duration of the pain?
- Is the pain experienced related to menstruation (period)?
- Is the patient breastfeeding?
- Has the patient previously had hormonal replacement therapy?
- Nipple discharge e.g. milk or something else?
- Colour of the discharge?
- Nipple unilateral or bilateral?
- Appearance changes of the nipple?
- Are there Lumps?
- Is there an abscess?
- When was the lump first noticed?
- Has the size increased or same size? Is it related to menstruation?
- Is there pain experienced in the lymph areas? Colour changes?
- Previous history of breast lumps.
- Amount of secretion of milk (galactorrhoea).
Additional questions may also be asked for differential diagnostic examination.
This approach is like men who are also at risk of breast cancer but have a lower incidence compared to women.
Has the size of the male breast tissue increased (gynaecomastia)?
Is it associated with drugs and anti-androgen medications?
In cases of prostate cancer, there is an examination called digital rectal examination (DRE). The aim is to detect the size of the prostate and the cause. There are four positions in which the patient can be examined in Figure 2: knee-chest, lithotomy (supine) lying on the back standing with the hips flexed and upper body supported by examining table, the left lateral with hips and knees flexed. The fourth position is bent over the table with legs apart, toes pointing inwards standing up (kneeling while resting on the elbow) (Nursingkey. n.d.). Adult males prefer left lateral and standing with hips flexed to observe the peranal and sacrococcygeal regions (Nursingkey, n.d.). The lithotomy position is preferred for women to do the rectovaginal examination. Transgender should be examined by their identified gender (Nursingkey, n.d.). A research study discovered that the supine is the preferred position for 53.9% of patients to better observe prostate characteristics (Furlan et al., 2008).

Figure 2: Positions performed during Digital Rectal Examination.
In the prostate gland, the posterior zone is close to the anterior rectal wall – please see Figure 3. This area is convex and the median sulcus divides the right and left lateral lobes. There is a third lobe that contains glandular tissue and is found between the ejaculatory duct and the urethra. The third or median lobe is not palatable on examination and contains secretory structures called alveoli that support the ejaculation fluid (Nursing Key, n.d.).
The gloved finger uses the right index finger and is rotated 360 degrees. The position of the clock facing 12 is the anterior side of the rectum and other features of a mass (Thomas and Monaghan, 2007).
The DRE is also used to examine for gastrointestinal cancers, for instance, anus and rectum (Thomas and Monaghan, 2007). The anal canal (anus) is about 2.5 to 4 cm long with a moist, hairless mucosa at the external margin. There is pigmentation in the perianal skin and the adult has hair present. There are two sets of concentric muscle rings called sphincters in the anus assessed during DRE. The sphincters are palpated for smoothness and evenness of pressure. Internal sphincters are smooth and are under involuntary nerve control. Upon maximal filling of the rectum with faeces (stools), it defecates and relaxes the internal sphincter. Defecation is controlled by the external sphincter voluntarily (Nursing Key, n.d.). Other examinations of the perianal area are for rashes, fissures, faecal soiling, blood, mucus, and anal warts. Irritation in the perianal area where fungal infection is more common in adults with diabetes whereas pinworm infestation is common in children (Nursing Key, n.d.)

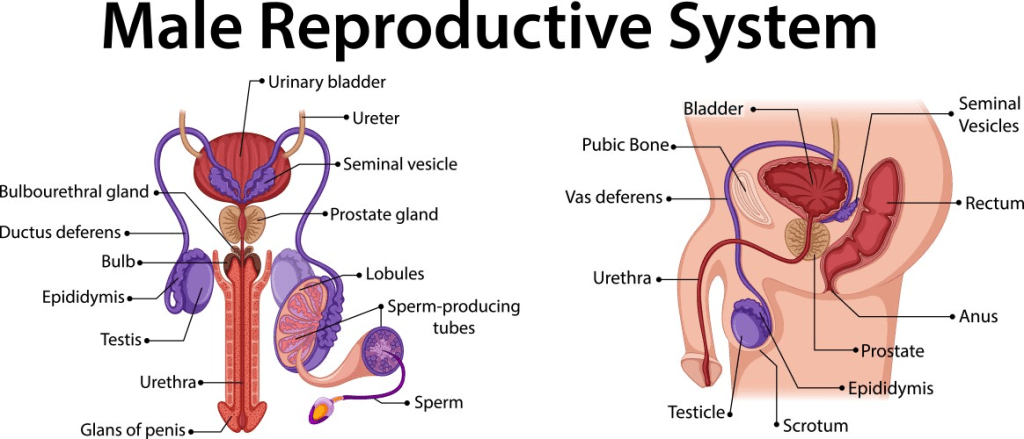
Figure 3: A) The different zones of the prostate gland B) Labelled structure of the male reproductive system with zones
There is variation in the texture of the prostate gland in normal and pathogen conditions. A normal prostate gland has a diameter of 4cm and feels firm, smooth, nontender, and slightly movable like a pencil eraser (Nursingkey, n.d.). Large abnormal size would indicate benign prostatic hyperplasia (Thomas and Monaghan, 2007). A benign prostate would feel smooth, partially soft, and symmetrical, and a central sulcus maintained (Nursing Key, n.d.). A rubbery consistency is felt and changes to being hard, and irregular, and loss of the central sulcus would be cancerous (Thomas and Monaghan, 2007). Inflammation of the prostate (prostatitis) is where the prostate gland is tender, and enlarged, and the body is warm (Thomas and Monaghan, 2007).
Many men dislike to undergo DRE (Furlan et al., 2008). Despite being cost-effective, fast, and high accessibility, there is a lack of awareness due to cultural prejudice. The DRE examination itself has limitations related to determining the prostate volume and initial detection of prostate cancer. However, the more experienced the physician, the smoother and the higher the sensitivity (Furlan et al., 2008).
Blood Tests
This can help check the patient’s general health and determine the symptoms experienced (Innes, 2009). Complete Blood Count (CBC) can help determine levels of red and white blood cells or the immune system for blood cancers such as leukaemia and lymphoma.
The blood test can also determine abnormal protein levels and tumour markers. Tumour markers are commonly proteins whose levels aid in diagnosis. It can help screen the general population but has low sensitivity and specificity (Lab Tests Online UK, 2023). Furthermore, not all tumours have an associated tumour marker. Elevated levels of one tumour marker occur for several tumours as presented in Table 1. High levels do not always indicate tumours. Therefore, clinical history, physical examination, and tumour markers must be used as part of a larger investigation in conjunction with imaging tests to diagnose cancer.
Table 1 Some of the main tumour markers used in cancer diagnosis (Lab Tests Online UK, 2023)
Urine Tests
Urine tests are a less invasive tool and provide information on bodily functions. They predominantly detect urological cancers such as bladder and kidney cancers. Gynaecological cancers are also detected like prostate and cervical cancers (Beer, 2019). Figure 4 presents a colour chart that assesses the urine to determine the hydration level. The darker or more concentrated urine colour signifies less hydration. There are two main ways in which cancer cells enter the urine: kidneys and bladder. The tubes that connect the kidney to the bladder is the ureter.
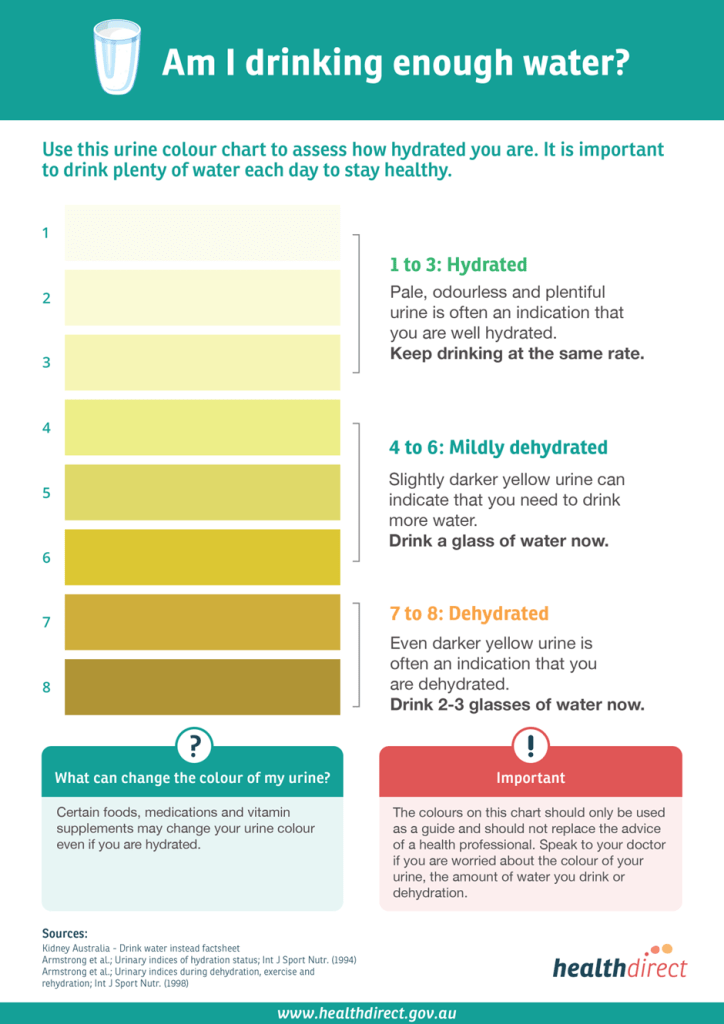
Figure 4 Urine colour chart.
Tumour markers can be detected in urine samples in cases of prostate cancer. Cells can also be scraped from the cervix, alimentary canal, and lungs using a spatula. They are then studied using the microscope to detect cancer and chronic inflammation; the laboratory technique is urine cytology – please see Figure 5. There are different types of urine specimens: voided, instrumented, and ileal conduit (Pansari, 2021). Voided urine is where three-second morning midstream urine samples are collected over three days in sequence for optimisation. Instrument urine is collected from a catheter whereas, ileal conduits are performed on patients who have undergone cystectomy. The ileum of the small intestine joins with the tubes that connect the kidney to the bladder called the ureter or the structure where pee (urine) leaves the body called the urethra. The Paris system is for reporting findings (Pansari, 2021).
Although this diagnostic tool causes lesser side effects and is easily obtainable, these groups of cells may not be representative of the whole tumour. Hence, biopsies tend to be more accurate and reliable.

Figure 5: A microscope image of low-grade urothelial carcinoma (transitional cell carcinoma of the bladder) that begins in the lining referred as urothelium in the urine with Papanicolau stain. It is a papillary cluster of malignant cells with nuclear pleomorphism, hyperchromasia (dark nucleus) and irregular nuclei borders. It has high nuclear to cytoplasmic ratio. It is negative for high grade urothelial carcinoma (NHGUC) (Reid et al., 2012; Pansari, 2021).
X-rays and scans
Depending on the symptoms that patients display, doctors propose the respective diagnostic tools. Correctly and accurately diagnosing cancer is vital for the prevention of unnecessary anxiety and the welfare of patients and their families. Several techniques have emerged to aid diagnosis and monitor the development of tumours and timely referral to treatment services (World Health Organisation, 2025).
Since some “lumps” cannot be physically felt, imaging the area of concern is often carried out. For example, if an abnormal mass grows deep within the breast tissue, it might not be felt upon physical examination. Hence, mammograms, i.e. X-ray examination of the breasts, are often suggested to pick up tumours in their early stages.
There are three important principles of imaging: detection, characterization, and monitoring of tumour to increase accuracy (Pulamati et al., 2023). Detection allows target areas to be seen to characterize the tumour. Characterization refers to defining the stage and determining the diagnosis and prognosis of the tumour. Monitoring allows observation of how the tumour is progressing and its impact on the body over time (Pulamati et al., 2023).
CT scan
A computerized tomography (CT) scan utilizes X-rays to create 3D images from different angles and a computer to create cross-sectional images similar to slices to see specific organs, bones, and blood vessels (Bryant, 2025). It helps to determine the size of the cancer and whether it spreads to other organs (MacMillan Cancer Support, 2022a). Pregnant women need to inform the healthcare professional. Preparative steps such as removal of any metal-containing objects on their body and being asked not to eat or drink for several hours (2 hours) before the scan (MacMillan Cancer Support, 2022a).
CT scans are more open and support patients if they experience anxiety – please see Figure 6. The use of contrast agents are either drunk or injected to help identify the target area in question more clearly and create a clear image: CT contrast commonly utilizes iodine for most patients excluding severe kidney disease and dehydrated patients who require special screening requirements/arrangements (Bryant, 2025). During the process, it makes them feel hot for a few minutes and the doctor needs to be informed before the procedure if the patient has asthma or an allergy to iodine to prevent serious reactions. The scan takes approximately 5 to 10 minutes but may stay longer in the department (MacMillan Cancer Support, 2022a).
The CT scan is used during emergencies because they are fast and accessible to detect trauma injuries such as fractures, haemmorhages (internal bleeding), lung conditions, and abdominal pain, and assess blood vessels (angiography) for heart conditions. It is useful to detect bones and air spaces for the chest, skeleton, and sinuses (Bryant, 2025)
CT scans are also commonly used to diagnose colorectal, stomach, head and neck, bone, ovary, and urological cancers. An example of a CT scan for liver cancer is in Figure 7. Amongst the advantages of CT scans are the speed preventing artifacts in the images, clear reconstructed radiographs of the cortical bone, and spatial information (space). However, there are limitations, for instance, radiation, less desirable imaging of soft tissues (suboptimal), and lack of functional information. To overcome this disadvantage, alternative imaging techniques are used functional magnetic resonance imaging (MRI) or Positron Emission Tomography (PET) (Pulmati et al., 2023).
In patients with brain cancers, CT and MRI can localize and guide the type of brain tumour. CT is useful for cancers in the brain stem and posterior fossa (Innes, 2009). Key examples are non-neural tumours of glial origin (astrocytoma, medulloblastoma, ependymoma). Ependymomas are common in both childhood and adults. Medulloblastoma and astrocytoma are common in childhood and young adults (Innes, 2009).

Figure 6: A CT scan

Figure 7: An CT image of liver cancer.
Positron Emission Tomography
This scan assesses the blood flow in particular areas of an organ that are active at a specified time using radioactive compounds e.g. glucose. Key examples of cancers detected are brain, cervical, oesophagus, head and neck, blood, thyroid, prostate, skin, lung, and breast (Pulmati et al., 2023). It is a useful diagnostic tool combined with CT to help provide functional and anatomical information and identify ‘missed’ cancerous lesions in conventional CT. However, some limitations include radiation exposure, spatial resolution, and detectability of cancerous lesions (Pulmati et al., 2023).
A recent study by Shawky et al. (2020) discovered that detected breast cancers had 100% sensitivity and 95.4% specificity under PET-CT examination compared to CT alone, where the sensitivity and specificity decreased to 81.2% and 90% respectively.
Similarly, there was a significant difference in Positive and Negative Predictive Value (PPV) and NPV). PPV presents patients who have been correctly diagnosed with positive results. NPV refers to patients who have been correctly diagnosed with negative results. The PPV for combined PET/CT (88.9%) was higher than CT alone (76.4%). The NPV for combined PET/CT (100%) is higher than CT alone (93%),
MRI scan
It is a scan that combines radio and magnetic waves to visualize the internal organ with detailed images. Common reasons to use the MRI scan are to determine whether the lump is cancerous, the size of the cancer, and whether it has metastasized (spread) post-surgery or when radiotherapy is required (Pulamati et al., 2023). An MRI scan of the brain tumour is in Figure 8. Other tumours used to diagnose via conventional MRI are prostate, primary bone, soft tissue sarcomas, bladder, spinal cord, and ovarian cancers (Pulamati et al., 2023). It can provide information on soft tissues that a CT scan cannot do. For example, the brain and spinal cord: strokes, nerve damage, and multiple sclerosis. Sports injuries in the muscles, tendons, ligaments, and joints. The abdomen and pelvis are seen more clearly, particularly the kidneys, prostate, liver, uterus, and ovaries. The structure and function of the heart are also assessed.
The scan lasts between 15 minutes and 1 hour. External metal objects must not be worn. Sounds are heard and earphones are given to listen to music during the scan. A gadolinium-based contrast dye is injected into the vein in the arm to improve the quality of the image and less likely to cause an allergic reaction (MacMillan Cancer Support, 2022b; Pulamati et al., 2023). Patients with chronic kidney disease require special screening and patients with pacemakers cannot have it due to magnet interference (Bryant, 2025). Other limitations are the MRI machine is enclosed, time-consuming, and expensive – Figure 9 (Pulamati et al., 2023).
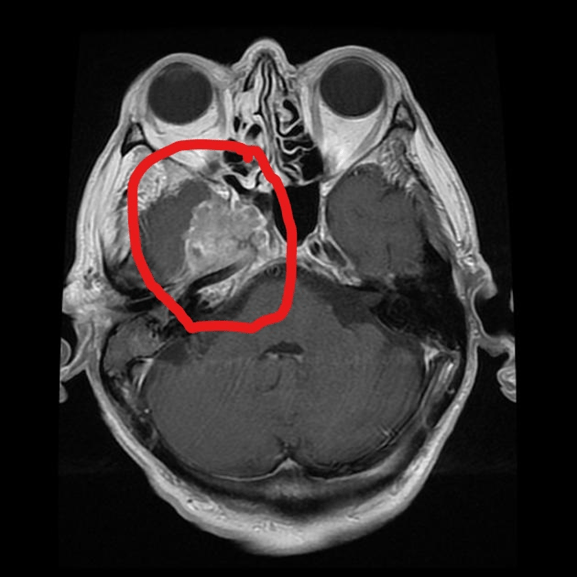
Figure 8: MRI scan of the brain. The tumour is marked with a red outline in an axial plane
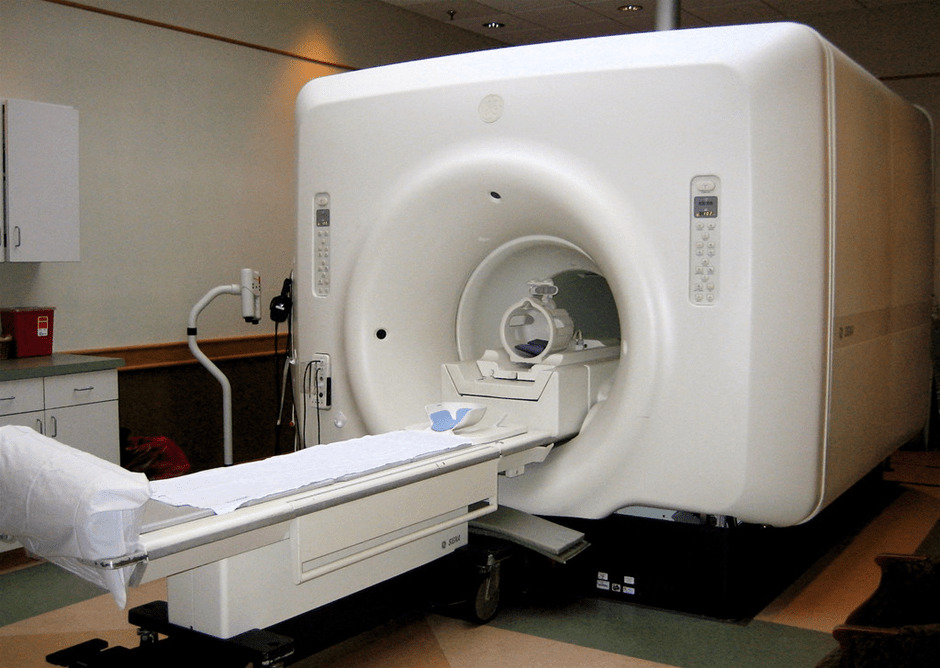
Figure 9: An MRI scanning maching.
Another form of magnetic resonance imaging is Magnetic Resonance Spectroscopy (MRS) and the mechanism differs from standard MRI. There are signals from compounds such as creatinine, lactate, N-acetyl aspartate, carbon, and hydrogen rather than water (Pulamati et al., 2023). MRS has shown great advantage in diagnosing cancer, for example, brain, breast, pancreatic, prostate, cervical, and gastrointestinal cancers (Pulamati et al., 2023).
Ultrasound
Ultrasound also known as sonogram uses sound waves with high frequency to create an image and can detect a range of cancers. For example, cysts or lumps can observed around the testicles or scrotum (the sac that holds the testes) for testicular cancer. It can help with neck examination of the lymph nodes in examining areas for suspected head and neck cancers. A gel is added onto the neck where the ultrasound probe or transducer moves around the area to produce sound waves as presented in Figure 10. These are transmitted to the computer device as a picture builds up. Samples of cells from the lump can be extracted using a fine needle. This process is called fine needle aspiration biopsy (MacMillan Cancer Support, 2022c).

Figure 10: Ultrasound image of the neck.
Endoscopy
This is a minimally invasive technique that allows an expert to “look” at some hollow structures in the body- this requires an instrument that videos the insides of an organ in real time. It is often used to observe the lungs, alimentary canal (including mouth, oesophagus, stomach, and intestines), urinary tract and female reproductive system.
For head and neck cancers, nasoendoscopy can examine the nose, mouth throat, and oesophagus and the use of anaesthesia is optional – please see Figure 11. An alternative called panendoscopy is performed more closely using a larger endoscope. In both types of endoscopy, an anesthesia spray is given, and instructed to not eat or drink for one to two hours until it goes. This helps to lower the risk of burning and swallowing the wrong way to the lungs via the trachea (windpipe) (MacMillan Cancer Support, 2022c). However, if the patient has allergies to anaesthesia, trans-nasal flexible laryngo-oesophagoscopy (TNFLO) is performed for analysis. The TNFLO endoscope passes through the nose; some patients can cope well and samples taken via biopsy may also occur. In all three cases, eating or drinking for several hours before the test is not permissible (MacMillan Cancer Support, 2022c).
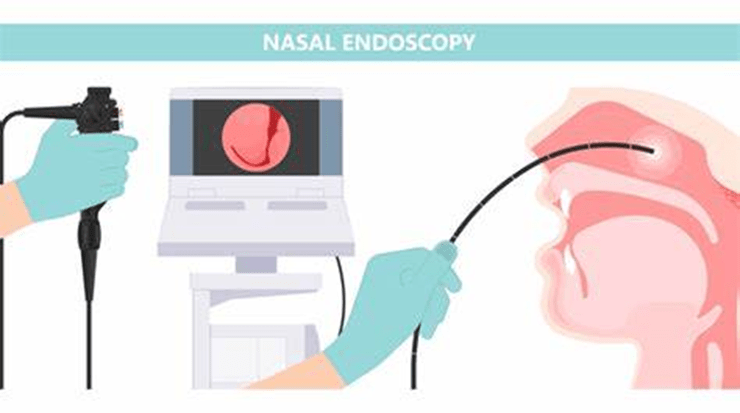
Figure 11: Nasoendoscopy
In other types of cancers, for instance, gastrointestinal cancers, endoscopy is a gold standard test. A thin tube passes through the back passage with a small camera to observe an organ of interest or the lining of the large bowel to determine if there are any polyps (non-cancerous growths). This test is called colonoscopy – please see Figure 12. Biopsies (removal of tissue) are also done for examination (Macmillan Cancer Support, 2025; Bowel Cancer UK, n.d). Flexible sigmoidoscopy observes the rectum and lower end of the large bowel called the sigmoid colon where polyps mainly occur – please see Figure 12 (Macmillan Cancer Support, 2024). Rigid sigmoidoscopy is an alternative to examine the rectum and anus.
Colon capsule endoscopy is a pill-like camera described as the size of a ‘large vitamin pill’ and is swallowed and images are sent digitally to the colonoscopist via a digital recording device in a small shoulder bag. It takes a day or two to enter the bowel (Bowel Cancer UK, 2021).

Figure 12: A range of diagnostic tests to detect bowel cancer.
Biopsy
In lieu of the invasive technique of biopsy, single or groups of cells can be studied under the microscope by a pathologist to make a definitive diagnosis of cancer. These cells or tissue samples of the abnormal lump or undefined growth are extracted from the brain or neck. There is a wide range of biopsies and depends on the type of tumour and location. Figure 13 presents key examples of biopsies used in lung cancer diagnosis. To further understand the nature of biopsy specimens, specialists can stain the samples using, for example, an H&E stain, which is equivalent to a dye. This “dye” stains cells in the samples to help understand the severity of the cancer. Different dyes used in conjunction to provide a holistic understanding of the tumour. It highlights the importance of imaging and tissue biopsy in cancer diagnosis where radiologists and pathologists communicate for combined knowledge to ensure the biopsy results are consistent with the radiological images to make a definitive diagnosis, and rational judgment on treatment planning.

Figure 13: Types of biopsies used for lung cancer diagnosis.
Staging And Grading Of The Tumour
The pathological staging of the tumour is part of cancer diagnosis because it describes the size and extent of the primary tumour (Tumour), the location and number of lymph nodes affected (N), and whether the tumour has metastasized/spread to other organs via the blood or lymph (M) at the time point of the surgery (National Cancer Institute, 2022). The TNM staging system can assist in cancer reporting as it allows physicians to understand the magnitude of the tumour, its potential course of action, and the administration of the right type of treatment.
Different staging systems depend on the type of cancer, for instance, the pancreatic staging system is presented in Figure 14 and has assigned individual scores. The T stage has Tis to T4, the N stage has Nx to N1 and the M stage has Mx to M1 (John Hopkins University, 2025). The information from the pathological stage and radiological imaging can develop a clinical staging. The lower the stage (pre-invasive) Stage 0-II, the better the long-term outcome compared to the higher stage (metastasis) Stage III-IV. Therefore, stage is a good prognostic factor to determine the right treatment (John Hopkins University, 2025).
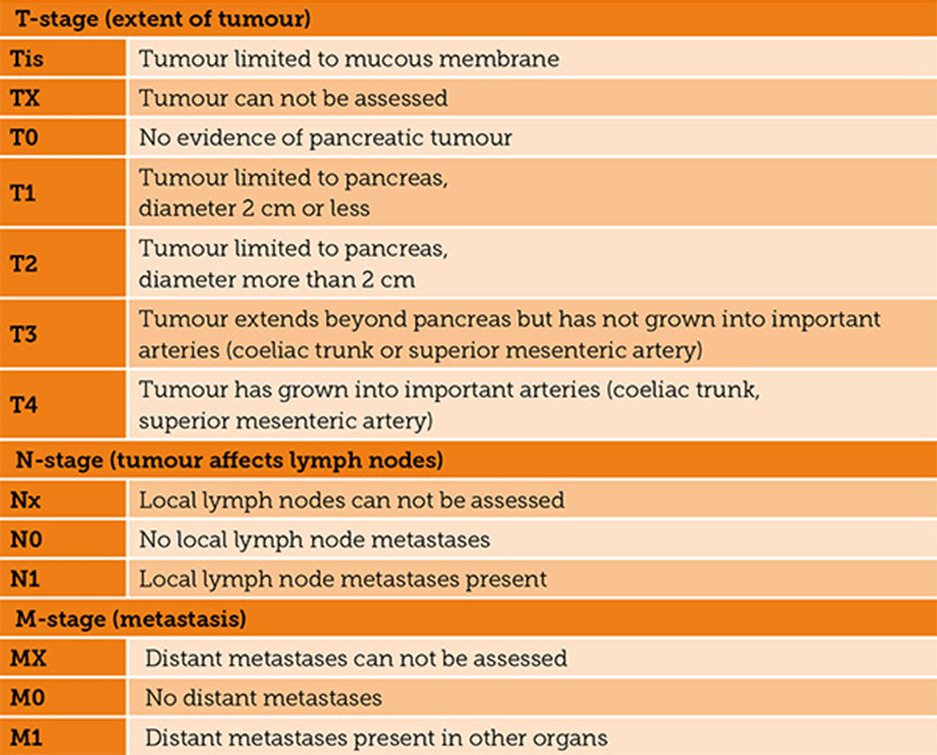
Figure 14: The TNM staging system for pancreatic carcinoma
Another staging method for cancers is predominantly used by cancer registries (National Cancer Institute, 2022). In situ, cancers are the presence of abnormal cells that have not spread to nearby tissue. Localized cancers are limited to the primary site. Regional cancers have spread to lymph nodes, organs, or tissues that are close by. Distant cancers have spread to organs at a far distance. Unknown status is insufficient information to confirm the stage (National Cancer Institute, 2022).
A grade is then assigned to the patient’s tumour and presents the likelihood that cancer can spread. For example, with low-grade tumours, surgical removal of the tumour might be sufficient for its eradication. Contrastingly, high-grade tumours might require a more targeted treatment, several sessions of chemotherapy, or certain types of drugs. For example, in cancers such as the breast, grading is in coordination with the Nottingham Histologic Score also known as the Elston-Ellis modification of the Scarff-Bloom-Richardson grading system (John Hopkins University, 2025). Three factors influence the scores: differentiation, pleomorphism, and mitotic count; each component has a score between 1 to 3. Differentiation refers to how well tumour cells are producing normal mammary glands. The pleomorphism refers to the features of the nucleus in the tumour cells. Mitotic count presents how active the cells are by mitosis (John Hopkins University, 2025). The total scoring range for Grade I tumours is between 3 and 5 and is less aggressive. Grade II tumours have a scoring range between 6 and 7 whereas, Grade III tumours have a scoring range between 8 and 9 and are more aggressive (John Hopkins University, 2025). An illustration of each grade and its respective features is in Figure 15.
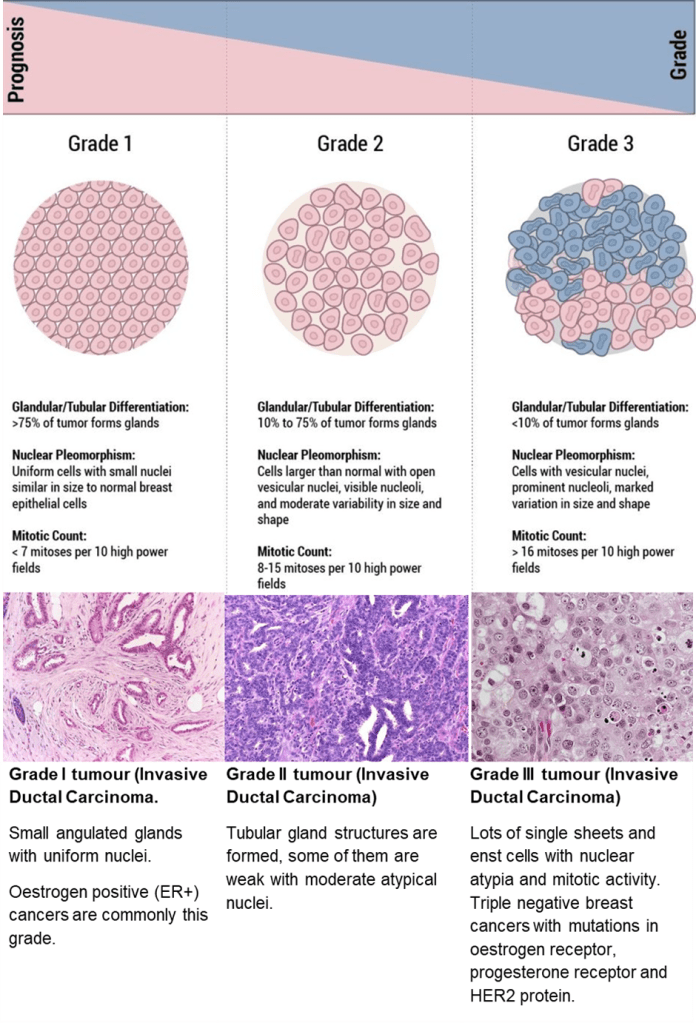
Figure 15: The grading system for breast cancer (John Hopkins University, 2025)
Screening
Screening helps identify specific cancers or precancerous lesions before symptoms develop. It is based on age and risk factors to avoid false positive results. Other cancers are more complex with specialized equipment and dedicated personnel. A positive test will lead to further tests to establish a definitive diagnosis and referral for treatment in timely intervals according to the Cancer Waiting Times (CWT). Patients who do not meet the age criteria for the screening programs and risk factors require alternative early diagnosis programs. The four main National Health Service screening programs are bowel, cervical, breast, and lung cancers.
Bowel Screening programme
Bowel cancer is the fourth most common cancer and the second causal factor in UK mortality. The screening program is aimed at patients aged 60 and 74 years where a home test kit is posted every two years to determine if there is blood in the faeces (poo). It helps lower mortality rates where 95% of people survived 5 years or more (Stockport Medical Group, n.d.). A flow diagram helps to give constructive feedback – please see Figure 16. Results are sent by post and, if the results are positive, further tests such as colonoscopy is required. However, if the results are normal, no further tests are needed and screening is repeated in two years (Stockport Medical Group, n.d.).
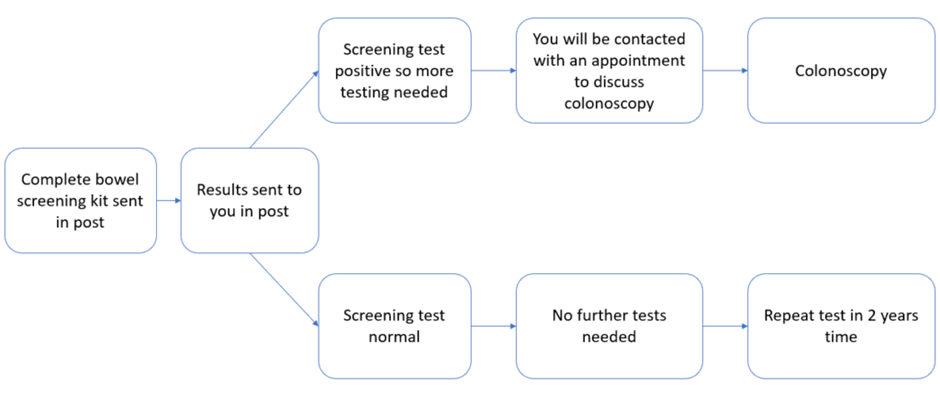
Figure 16: Diagnostic pathway for the Bowel Screening programme (Stockport Medical Group (n.d.)
Please click the link below for further information on NHS bowel screening.
Breast Screening Program (mammography)
This screening program is for women aged 50 to 71 years and invited every three years (Martin, 2024). There are two types of mammograms: diagnostic and screening. The diagnostic mammogram helps to diagnose breast cancer if there are suspicious lumps, nipple discharge, pain and thickness in the brain, variation in both breast size and shape, and other breast abnormalities. In contrast, a screening mammogram consists of two X-ray images of the breast for patients with unsuspected breast cancer who are asymptomatic (no symptoms) and do not have small calcifications. Therefore, screening of the breast helps to differentiate between benign and malignant breast cancer and evaluate the symptoms and effectiveness of radiation. If the removal of one breast is performed via mastectomy, the other breast or lateral should accompany her or him for support. Palpitations of breast masses are also examined (Martin, 2024; National Health Service, n.d.)
Please click the link below for further information on NHS breast screening.
Cervical Cancer screening program.
Cervical screening otherwise known as smear test observes the cervix of the female reproductive system and helps prevent cervical cancer. A small sample of cells undergo microscopic evaluation to determine types of human papillomavirus (HPV). The two predominant HPV types 16 and 18 are associated with cervical cancer – please see Figure 17. Other HPV infections can occur during sexual intercourse (vagina, oral or anal), skin contact, and other methods. However, having the HPV vaccine, hygiene, one spouse, or not having sexual intercourse for a long time does not lower the risk but can contribute to preventative measures. Other reasons for infection may be associated with the same partners, trans, not having sexual intercourse for age, or surgery (partial hysterectomy) to not halt the cervix (National Health Service, n.d). HPV DNA and mRNA are also detected by molecular tests.

Figure 17: Flowchart presenting how to deal with negative and positive results for cervical cancer screening (National Health Service, n.d.)
Please click the link below for further information on NHS cervical screening.
Lung Cancer screening program.
Lung cancer has a higher mortality rate than other cancers in the UK with no signs or symptoms of early-stage cancers before they arrive to make treatment more successful. Patients aged 55 to 74 years who have smoked are invited for a lung health check. The UK government has initiated in certain areas in England where it will be more predominant all over the UK by 2029 (National Health Services, 2023). The screening aims to examine the lung function and the healthcare professional will be asked about lifestyle, breathing, family history, height, weight, and clinical history (National Health Services, 2023).
There are three possible outcomes post-consultation: no further action, referral to a general practitioner (GP), and a CT scan. No further action means there is a low probability or risk of developing lung cancer and, no further steps are required. A referral to a GP is made if breathing difficulties arise and can be discussed in detail. However, if all treatment strategies and suggestions have not worked, the GP may refer the patient to a respiratory specialist for further investigation. A CT scan is organized and performed on the same day or booked as another appointment if the patient is deemed at high risk of developing lung cancer to get a clear image of the lungs. Patient notes and appointments are sent electronically to the GP with details and reasoning (National Health Service, 2023).
Please click the link below for further information on NHS Lung screening.
New Diagnostic Techniques
National Institute for Health and Care Research (2025) announced a new cutting-edge experimental blood test that can detect six types of early-stage cancer via circulating DNA in the blood: colorectal, oesophageal, pancreatic, renal, ovarian, and breast compared to wild-type/non-cancer patients. The test is a type of liquid biopsy called TriOx with a high sensitivity (94.9%) and moderately high specificity (88.8%). The current ethos is to develop and validate the test with additional cancer types and larger cohorts of patients to make it similar to a routine blood test or checking blood glucose levels.
Liquid biopsy is a novel, minimally invasive diagnostic technique that utilizes bodily fluids. For instance, blood, urine, or saliva, to detect molecular markers for solid malignancies: circulating tumour cells (CTC), circulating or free microRNA, and circulating tumour DNA (ctDNA). This helps to diagnose and monitor progress and is useful in personalized medicine for effective cancer care management (Pulamati et al., 2023).
Next-generation sequencing (NGS) can analyze the genetic and epigenetic changes of ctDNA to detect cancer early and be involved in tumour staging, prognosis, and response to chemotherapy or surgery (Pulamati et al., 2023). NGS can also detect genetic mutations in DNA regions that do not code for proteins and are transcribed into long non-coding RNA (lncRNAs) and contribute to the hallmarks of cancer.
Similarly, exosomes are extracellular vesicles and are another minimally invasive tool found in bodily fluids: urine, saliva, breast milk, and plasma. It has good stability and is secreted from body cells that carry RNA, DNA, metabolites, and lipids involved in cellular communication. If these cells have genes and or protein changes in their structure or function, exosomes can be used as a biomarker in bodily fluids to detect cancer early (Pulamati et al., 2023).
Conventional colposcopy is a gold standard test for cervical cancer. However, Artificial intelligence (AI) can guide colposcopy in developed and undeveloped countries to prevent the risk of cervical intraepithelial neoplasia (CIN) where features can be recognized by deep learning algorithms in digital colposcopy images. This helps lower costs, improve quality of care, and improve connections between primary, secondary, and tertiary care services in developed and undeveloped countries (Pulamati et al., 2023).
.
Overall, the cancer diagnostic pathway has multiple steps to enable early detection rates. It begins with a physical examination for abnormalities in different anatomical sites, laboratory investigations e.g. blood and urine tests, followed by radiological imaging and staging. Screening programs are strongly dependent on the rate of accurately identifying the lesions for early treatment to prevent tumour progression. Various technological advancements for new opportunities to improve clinical management, particularly in undeveloped countries (Pulamati et al., 2023).
References
Beer, G. (2019) Urine Tests: Detecting Cancer in the Pee. Available at: https://news.cancerresearchuk.org/2019/11/21/urine-tests-detecting-cancer-in-pee/ (Accessed: 17th April 2025)
Bowel Cancer UK (n.d.) Going for a colonoscopy. Available at: https://www.bowelcanceruk.org.uk/about-bowel-cancer/diagnosis/hospital-tests/going-for-a-colonoscopy/ (Accessed: 18th April 2025)
Bryant, A. (2025) CT Scan vs. MRI: Understanding the Key Differences and When to Use Each Available at: https://www.rupahealth.com/post/ct-scan-vs-mri-understanding-the-key-differences-and-when-to-use-each (Accessed: 17th April 2025)
Cancer Research UK (2021) Patients invited to swallow a tiny camera to look for signs of bowel cancer. Available at: https://www.bowelcanceruk.org.uk/news-and-blogs/research-blog/patients-invited-to-swallow-a-tiny-camera-to-look-for-signs-of-bowel-cancer/ (Accessed: 18th April 2025)
Cancer Research UK (2022) Signs And Symptoms of Cancer. Available at: https://www.cancerresearchuk.org/about-cancer/cancer-symptoms (Accessed: 18th April 2025)
Furlan, A.B., Kato, R., Vicentini, F., Cury, J., Antunes, A.A. and Srougi, M. (2008). Patient’s reactions to digital rectal examination of the prostate. International Brazilian Journal of Urology, 34(5), pp.572–576. doi:https://doi.org/10.1590/s1677-55382008000500005.
Innes, A. (2009) Davidson’s Essentials of Medicine. London: Elsevier
John Hopkins University (2025) Staging and Grade. Available at: https://pathology.jhu.edu/breast/staging-grade/ (Accessed: 18th April 2025)
Lab Tests Online UK (2023) Tumour Markers Available at: https://labtestsonline.org.uk/tests/tumour-markers (Accessed: 17th April 2025)
MacMillan Cancer Support (2022a) CT scans https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/ct-scan (Accessed: 17th April 2025)
MacMillan Cancer Support (2022b) MRI scans https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/mri-scan (Accessed: 17th April 2025)
MacMillan Cancer Support (2022c) Head and Neck Cancer tests https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/tests-for-head-and-neck-cancer (Accessed: 18th April 2025)
MacMillan Cancer Support (2024) Sigmoidoscopy. Available at: https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/sigmoidoscopy-for-bowel-cancer (Accessed: 18th April 2025)
MacMillan Cancer Support (2025) Colonoscopy. Available at: https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/colonoscopy (Accessed: 18th April 2025)
Martin, P. (2024) Mammography (Mammogram) Available at: https://nurseslabs.com/mammography-mammogram/ (Accessed: 18th April 2025)
National Cancer Institute (2022) Cancer Staging Available at: https://www.cancer.gov/about-cancer/diagnosis-staging/staging (Accessed: 18th April 2025)
National Health Service (2023) Lung cancer screening Available at: https://www.nhs.uk/conditions/lung-cancer-screening/ (Accessed: 18th April 2025)
National Health Service (n.d.) Breast Screening (mammogram) Available at: https://www.nhs.uk/conditions/breast-screening-mammogram/ (Accessed: 18th April 2025)
National Health Service (n.d.) Cervical Cancer Screening Available at: https://www.nhs.uk/conditions/cervical-screening/ (Accessed: 18th April 2025)
National Institute for Health and Care Research (2025) New blood test shows promising potential for early cancer detection. Available at: https://www.nihr.ac.uk/news/new-blood-test-shows-promising-potential-early-cancer-detection (Accessed: 17th April 2025)
Nurse Key (2020) Anus, Rectum and Prostate. Available at: https://nursekey.com/anus-rectum-and-prostate-2/ (Accessed: 18th April 2025)
Pansare, V. (2021) Bladder & urothelial tract Cytology Paris system for urothelial neoplasia. Available at: https://www.pathologyoutlines.com/topic/bladdercytologyparissystemnew.html (Accessed: 18th April 2025)
Pulumati, A., Pulumati, A., Dwarakanath, B.S., Verma, A. and Papineni, R.V.L. (2023). Technological advancements in cancer diagnostics: Improvements and limitations. Cancer Reports, [online] 6(2). doi:https://doi.org/10.1002/cnr2.1764.
Reid, M.D., Osunkoya, A.O., Siddiqui, M.T. and Looney, S.W. (2012). Accuracy of grading of urothelial carcinoma on urine cytology: an analysis of interobserver and intraobserver agreement. International Journal Of Clinical Experimental Pathology 5(9):882-91
Shawky M, Ali ZAE, Hashem DH, Houseni M. Role of positron‐emission tomography/computed tomography (PET/CT) in breast cancer. Egypt J Radiol Nucl Med. 2020;51(1):125.
Shawky, M., Ali, Z.Y., Hashem, D.H., and Houseni, M. (2020). Role of positron-emission tomography/computed tomography (PET/CT) in breast cancer. Egyptian Journal of Radiology and Nuclear Medicine. 51(1) p. 125 doi:https://doi.org/10.1186/s43055-020-00244-9.
Stockport Medical Group (n.d.) NHS Bowel Cancder Screening. Available at: https://www.stockportmedicalgroup.nhs.uk/help-support/nhs-screening/nhs-bowel-cancer-screening/
Thomas, J. and Monaghan, T. (2007) Oxford Handbook Of Clinical Examination And Practical Skills Oxford: Oxford University Press.
World Health Organisation (2025) Cancer. Available at: https://www.who.int/news-room/fact-sheets/detail/cancer (Accessed: 16th April 2025)
Leave a comment