New Research Into the Causes And Treatment Of Head And Neck Cancer
New Research One: Pembrolizumab increases survival rates
Researchers at the Institute of Cancer Research (2025) have developed more effective immunotherapy drugs to treat Head and Neck Cancer, aiming to improve quality of life.
Pembrolizumab extends life by three years with advanced disease.
From one of their clinical trials, they discovered that Pembrolizumab is a first-line treatment for recurring cancers and has better survival rates compared to standard chemotherapy.
Mode of Action of Pembrolizumab By Drugs.com
Mode of Action of Pembrolizumab By Hypertunity
New Research Two: Nivolumab increases survival rates
Researchers from The Institute of Cancer Research (2025) discovered that Nivolumab increases survival rates by three times in patients with advanced head and neck cancer. Hence, in 2017, they were given to patients who were receiving chemotherapy, yet their head and neck cancer progressed within six months.
Mode of Action of Nivolumab By Drugs.com
Mode of Action of Nivolumab By Inevid
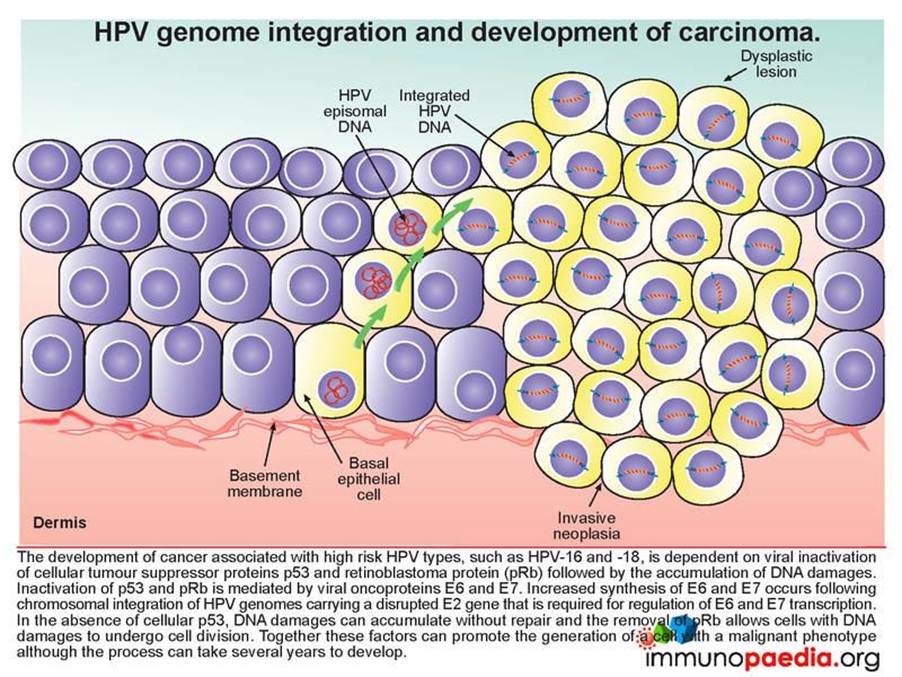
New Research Three: HPV Blood Test
Human Papillomavirus (HPV) is a risk factor for head and neck cancer. Researchers from the Institute of Cancer Research (2025) and Royal Marsden created a blood test that helped:
- To determine whether patients with HPV-positive head and neck cancer will have residual tumours after treatment with chemotherapy and radiotherapy.
- To determine which patients would respond better to treatment to prevent unnecessary treatment.
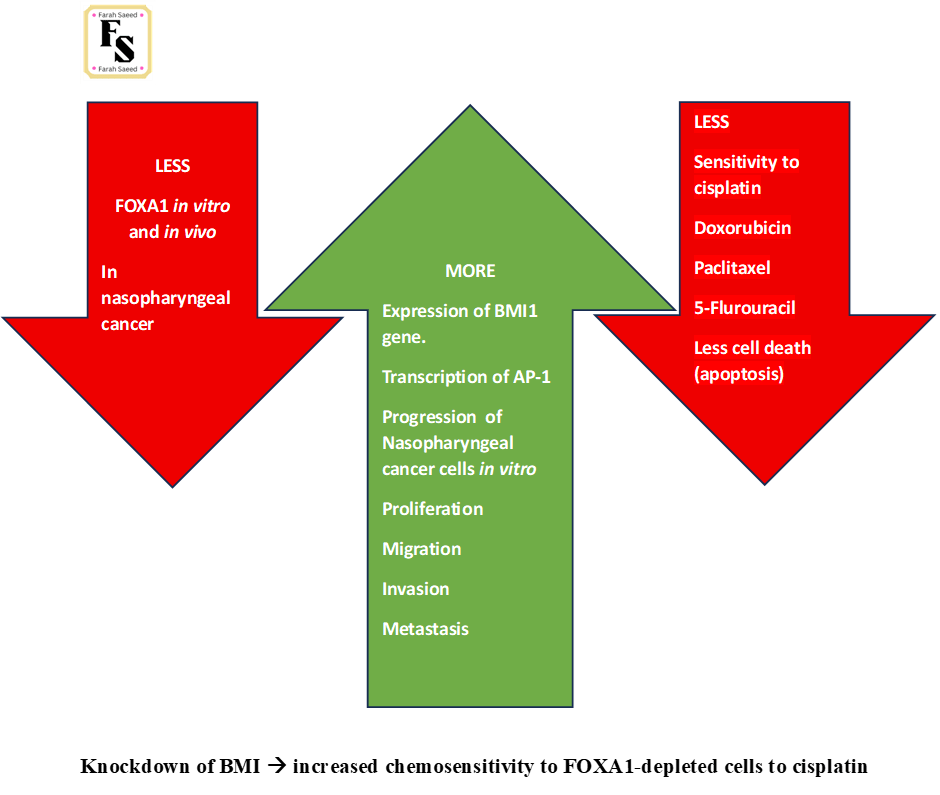
New Research Four: FOXA1 and BMI1
Qin et al. (2025) discovered there is an inverse relationship between the transcriptional regulator Forkhead Box A1 (FOXA1) and B-cell-specific Moloney murine leukaemia virus integration site 1 (BMI1) in patients with nasopharyngeal cancer.
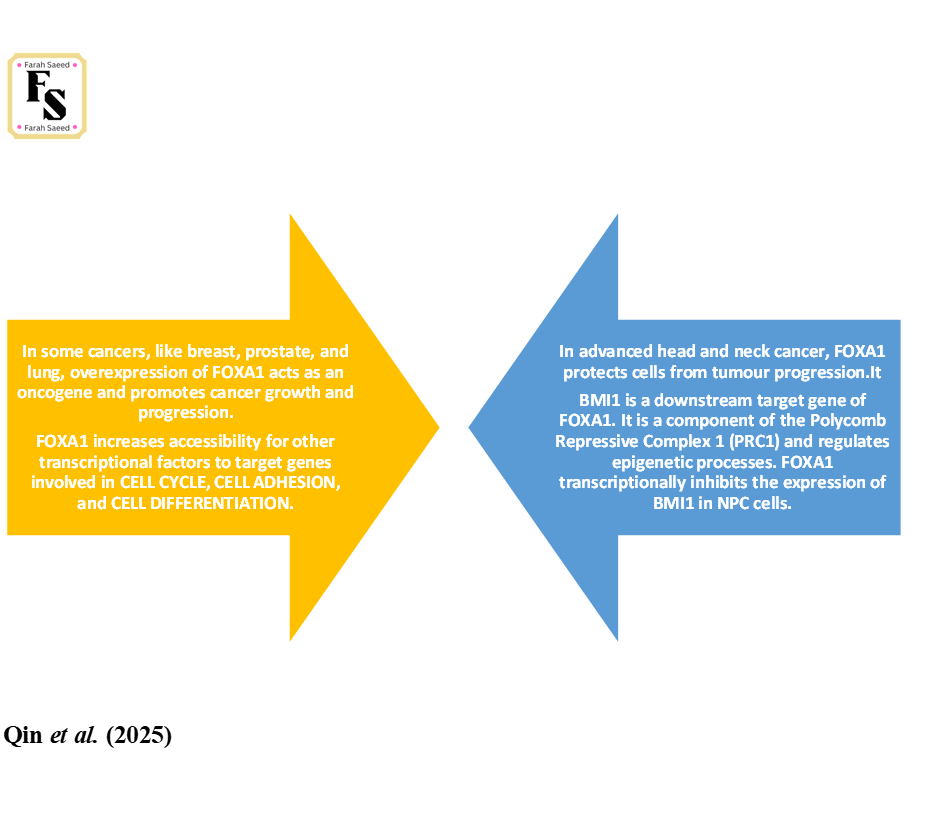
FOXA1 inversely correlated with WHO classification and TNM staging (Qin et al., 2023).
Low FOXA1 expression linked to higher TNM staging and higher grades 3 and 4 (III-IV)
Tumour sizes (T3-T4)
Lymph node (N2-N3)
Metastasis (M1)
FOXA1 and BMI1 have opposing effects on the PI3K/Akt pathway despite their share effects Akt and modulate overlapping gene targets.

BMI increases tumour aggressiveness and chemoresistance opposing FOXA1 by activating PI3K/Akt signaling.
FOXA1 suppresses MND1 promoter to inhibit cancer progression and increase sensitivity of oxaliplatin in the PI3K/Akt pathway (Hu et al., 2023)
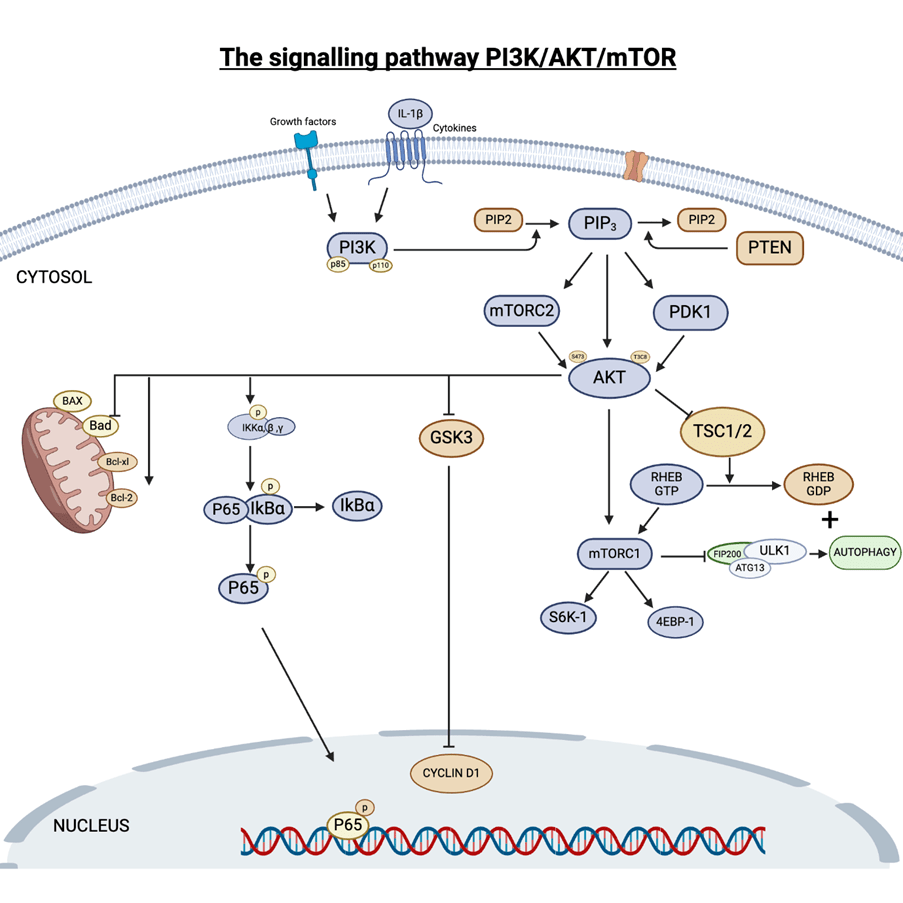
The normal PI3K/AKT/mTOR signalling pathway responds to sugar (glucose), hormones (insulin) and growth hormones) that activates downstream Akt mTORC and control cell cycle and autophagy (Upadhyay, 2025)
References
Hu, X., Zhou, S., Li, H., Wu, Z., Wang, Y., Meng, L., Chen, Z., Wei, Z., Pang, Q. and Xu, A. (2023). FOXA1/MND1/TKT axis regulates gastric cancer progression and oxaliplatin sensitivity via PI3K/AKT signaling pathway. Cancer Cell International, 23(1). doi:https://doi.org/10.1186/s12935-023-03077-4.
Qin, Y., Yang, M., Cao, Y., Fu, Y., Yang, F., Zhang, X. and Xiao, S. (2025). Targeting the FOXA1/BMI1 axis to overcome chemoresistance and suppress tumor progression in nasopharyngeal carcinoma. Cell Death Discovery, 11(1). doi:https://doi.org/10.1038/s41420-025-02595-6.
The Institute of Cancer Research (2025) Our research into head and neck cancer. Available at: https://www.icr.ac.uk/research-and-discoveries/types-of-cancer/head-and-neck-cancer (Accessed: 25th July 2025)
Upadhyay, A. (2025) The PI3K/AKT/mTOR signalling pathway. Available at: https://www.biorender.com/template/the-pi3kaktmtor-signalling-pathway (Accessed: 25th July 2025)