
Types Of Testicular Cancer
The tumour tissue consists of cancer cells with diverse molecular backgrounds alongside stromal cells that surrounds the tissue. This is referred as intra-tumoural heterogeneity where the tumour microenvironment is different to normal phenotype and can adaptations contributes to loss or degeneration of the tissue (hypotrophy) and hypoxic conditions (Hanahan and Weingberg, 2011).
GNIS-related tumours
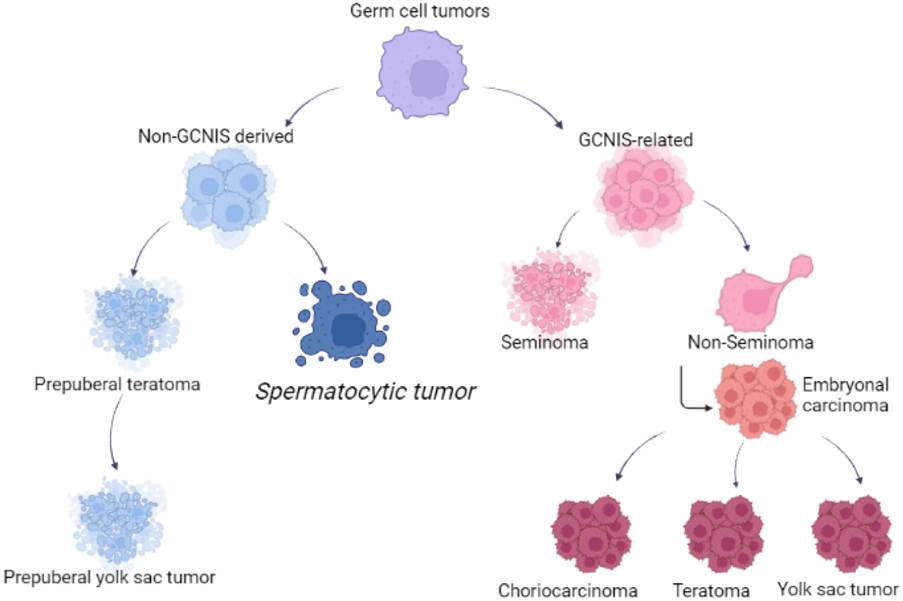
GNIS-related tumours arise when gonocytes do not differentiate into spermatogonia and form intratubular germ cell neoplasia. They can become invasive until puberty age when changes in the levels of hormones occur (Rajpert-De Meyts, 2006). They represent 95% of testicular cancer cases and are subdivided into Seminomas and non-seminomas.
Seminomas
Seminomas are slow-growing tumours that arise in mutated germ cells that block the differentiation from gonocytes to spermatogonia (American Cancer Society, 2018; Gaddam, Bicer, and Chestnut, 2023). More than 95% of cases are classical and commonly occur in young males aged 25 to 45. They can progress onto the lymph nodes. They are sensitive to both radiotherapy and chemotherapy and are associated with better outcomes (prognosis).
Non-Seminomas
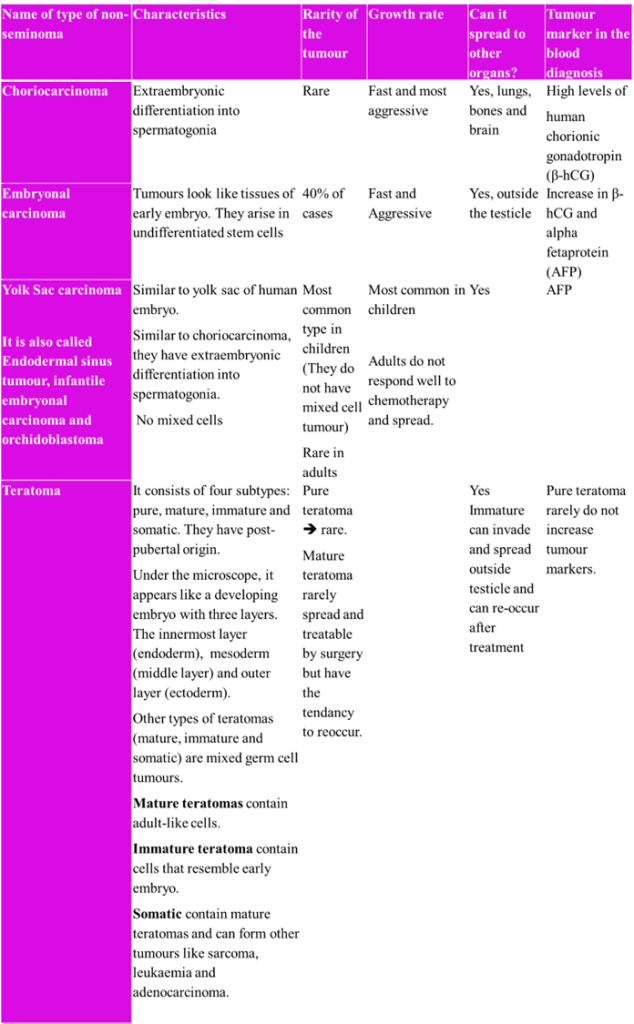
Non-seminomas are fast-growing tumours and are the most common type of testicular cancer (Cancer Research UK, 2025a). Patients between the late teenagers and early 30s are at risk. They contain more than one cell type (mixed cell tumors) and are not sensitive to radiation therapy but are sensitive to chemotherapy. Non-seminomas can become more aggressive and can spread to the retroperitoneal lymph nodes (American Cancer Society, 2018). Therefore, accurate diagnosis improves outcomes.
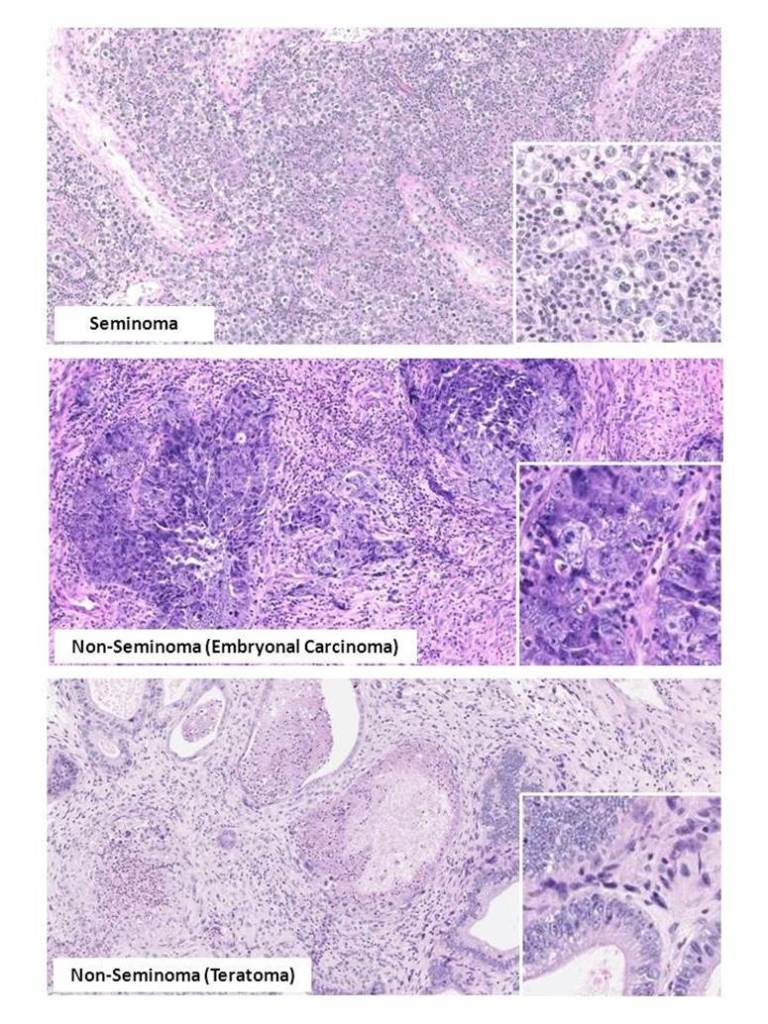
Histological images of GNIS-related tumours stained with Haemoxylin-Eosin stain (Endotext, 2014). A) seminoma B) embryonal carcinoma (non-seminoma) C (teratoma (non-seminoma). The square provides greater magnification to differentiate between them.
A summary table has been designed based on several research papers (American Cancer Society, 2018; Roland, 2024; Gaddam, Bicer and Chestnut, 2023).
Non-GNIS-related tumours
Spermatocytic tumour.
Spermatocytic cancer is an example of a non-GNIS tumour. It is derived from postpubertal-type germ cells (Secondino et al., 2023). Spermatocytic tumours are less common and occur in older males (American Cancer Society, 2018). They do not grow beyond the testicles (Roland, 2024). Spermatocytic cancers are characterized as having a unilateral mass, some researchers have reported bilateral mass (Secondino et al., 2023). The tumour size has been estimated to be between 2 and 20 cm with an average of 7 to 8 cm.
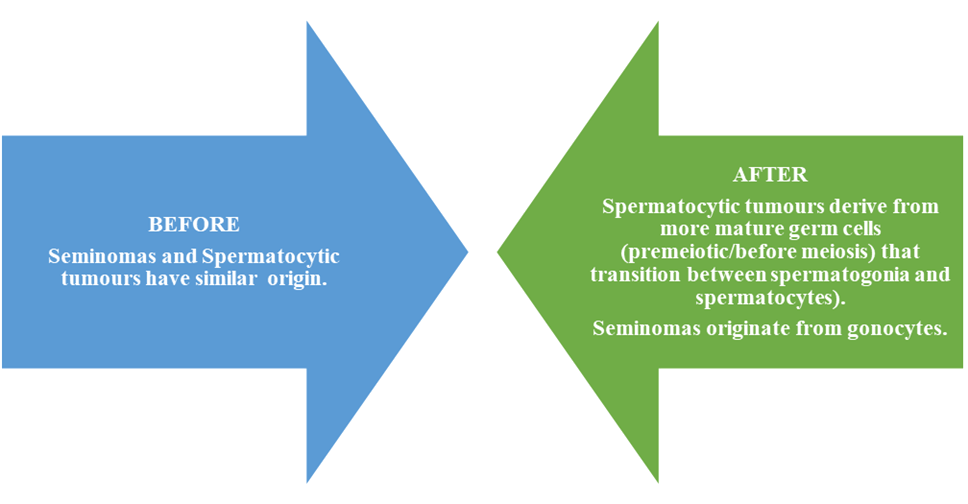
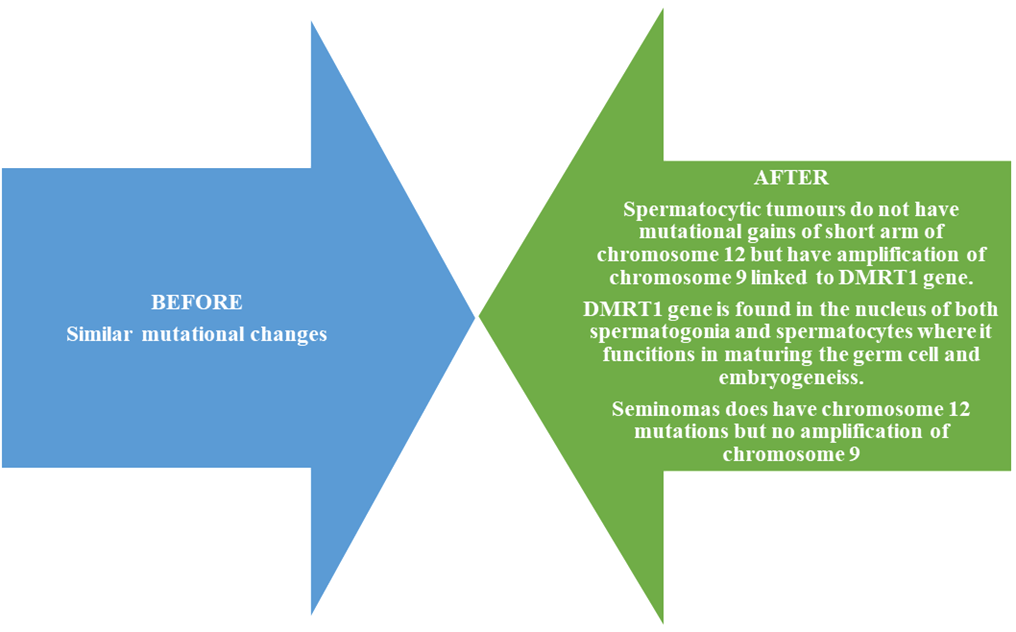
It was originally thought to be a subtype of GNIS-related cancers like seminoma because it closely resembled spermatogonia with large-sized tumours (Secondino et al., 2023). Masson (1946) referred to it as ‘le seminoma spermatocitaire’. However, spermatocytic tumours are less likely to have more than Stage 2 and 16.4% of cases are smaller than 3cm. In contrast, there are more cases of seminomas (27.6%) that have cancers smaller than 3cm (Secondino et al., 2023).
Changes to World Health Organisation Classification of Testicular Cancers 2016
(Secondino et al., 2023)
References
American Cancer Society (2025) What’s New in Testicular Cancer Research? Available from https://www.cancer.org/cancer/types/testicular-cancer/about/new-research.html (Accessed: 3rd July 2025)
Boccellino, M., Vanacore, D., Zappavigna, S., Cavaliere, C., Rossetti, S., D’Aniello, C., Chieffi, P., Amler, E., Buonerba, C., Di Lorenzo, G., Di Franco, R., Izzo, A., Piscitelli, R., Iovane, G., Muto, P., Botti, G., Perdonà, S., Caraglia, M. and Facchini, G. (2017). Testicular cancer from diagnosis to epigenetic factors. Oncotarget, 8(61), pp.104654–104663. doi:https://doi.org/10.18632/oncotarget.20992.
Cancer Research UK (2025a) Types of testicular cancer. Available at: https://www.cancerresearchuk.org/about-cancer/testicular-cancer/types (Accessed: 3rd July 2025)
Endotext (2014) Testicular Cancer: Pathogenesis, Diagnosis and Management with Focus on Endocrine Aspects Available at: https://www.endotext.org/chapter/testicular-cancer-pathogenesis-diagnosis-and-endocrine-aspects/fig-2-4/ (Accessed: 3rd July 2025)
Gaddam, S.J., Bicer, F., Chesnut, G. (2023) Testicular Cancer. Available at: https://www.ncbi.nlm.nih.gov/books/NBK563159/ (Accessed: 3rd July 2025)
Hanahan, D. and Weinberg, Robert A. (2011). Hallmarks of cancer: the next Generation. Cell, 144(5), pp.646–674. doi:https://doi.org/10.1016/j.cell.2011.02.013.
Macmillan Cancer Support (2022) Testicular cancer and the lymph nodes. Available at: https://www.macmillan.org.uk/cancer-information-and-support/testicular-cancer/lymph-nodes (Accessed: 3rd July 2025)
Masson, P. (1946) A study of seminomas. Annual Review of Cancer Biology, 5, pp. 361–387.
Rajpert-De Meyts, E. (2006) Developmental model for the pathogenesis of testicular carcinoma in situ: genetic and environmental aspects. Human Reproduction Update 12(3): pp.303-23
Roland, J. (2024) What Are the Different Types of Testicular Cancer?. Available at: https://www.healthline.com/health/cancer/testicular-cancer-types (Accessed: 3rd July 2025)
Secondino, S., Viglio, A., Neri, G., Galli, G., Faverio, C., Mascaro, F., Naspro, R., Rosti, G. and Pedrazzoli, P. (2023). Spermatocytic Tumor: A Review. International Journal of Molecular Sciences, [online] 24(11), p.9529. doi:https://doi.org/10.3390/ijms24119529
Leave a comment