
Diagnosis of TesticularCancer
Self-Diagnosis
Self-examination of the testicles takes no more than 10 minutes to perform and can save a life! Try to do this every three month and if you are able to make it a regular habit, every month! (Check4Cancer, 2021.
What do you need: Hot shower, soap, hands and eyes.
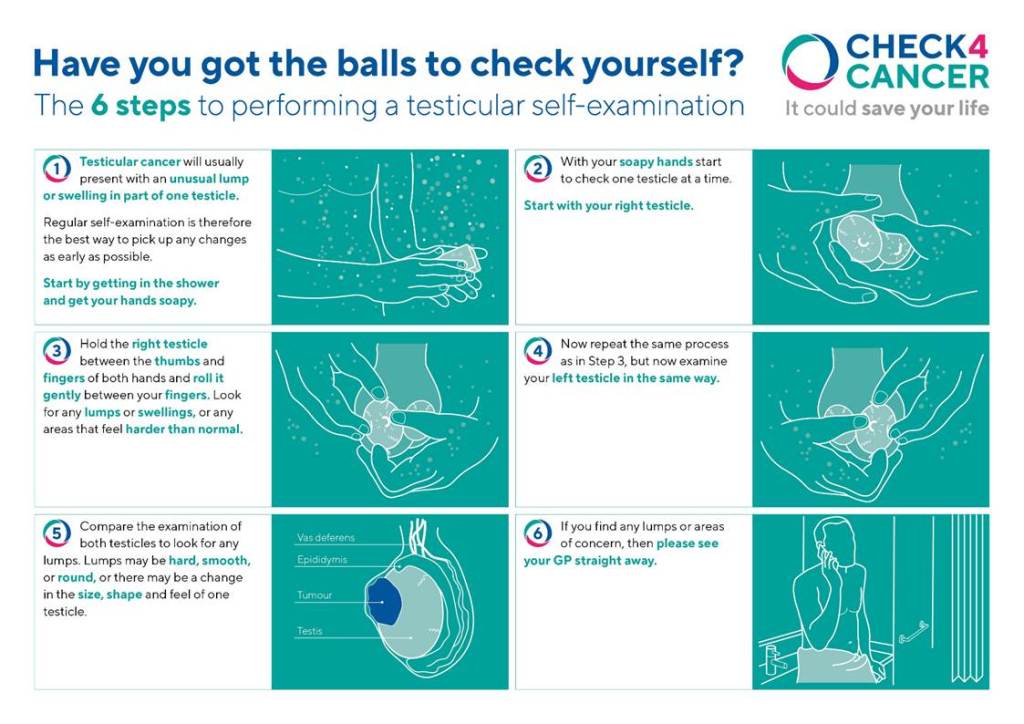
(Check 4 Cancer, 2021)
Are You An Auditory Learner?
Please have a look at this video
For further guidance on how to check the testicles, please visit MacMillan Cancer Support:
https://www.macmillan.org.uk/cancer-information-and-support/testicular-cancer/how-to-check
Staging systems of Testicular Cancer

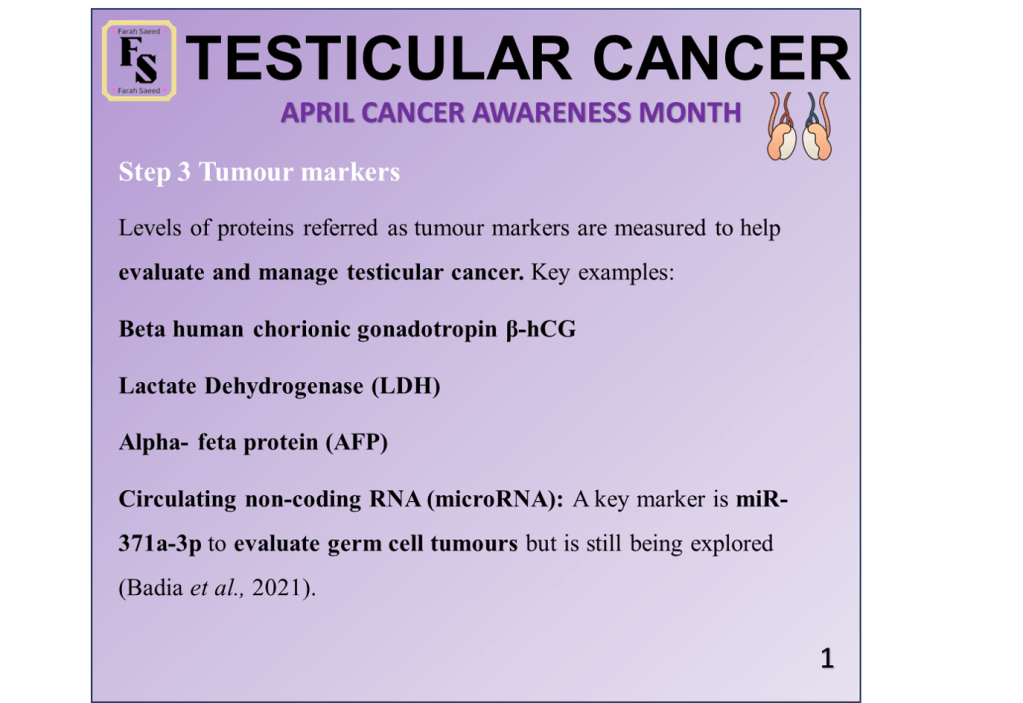
Examples Of Tumour Markers
Levels Of Tumour Markers Within The Staging System
S0 refers to the tumour marker levels being normal.
S1 suggests the tumour marker levels are slightly high.
S2 indicates the tumour marker levels are intermediate.
S3 signifies that the levels of the tumour markers are very high.
However, it does not follow the same concept as staging.
For instance, in Stage 0, you have S0, and in Stage 3, you have S3 –> INCORRECT
Instead…
In early-stage testicular cancers,
Stage 1 cancer is subdivided into Stage 1A and Stage 1 B.
Stage 1A – cancer within the testicles only
Stage 1B – cancer is outside the testicle but has not spread to the lymph nodes.
In both stages, the tumour markers are normal (S0).
However, in Stage 1S – This suggests that a minimum of ONE of the tumour markers is raised as S1, S2, or S3.
On the other hand, in late-stage testicular cancers,
In Stage 3, cancer is subdivided into: 3A, 3B, and 3C.
Stage 3A suggests the cancer has spread to the lymph nodes at distant sites and the lungs. The tumour markers are normal (S0) or slightly raised (S1).
Stage 3B has TWO outcomes:
It signifies the cancer is in the lymph nodes near the tumour, where the markers are at an intermediate level (S2)
OR
The lungs are affected alongside the distant lymph nodes with tumour markers at S2.
Stage 3C also has TWO outcomes:
It can be similar to Stage 3B; however, the tumour marker level is high S3
OR
The tumour has spread to other organs, for instance, the liver or brain, but the level of the tumour markers can be: S0, S1, S2, or S3.
Please click here to visit Cancer Research UK understand more about the staging system of testicular cancer
https://www.cancerresearchuk.org/about-cancer/testicular-cancer/stages-tnm
TNM staging system of UICC
The 2016 Tumour, Node, Metastasis (TNM) classification of the International Union Against Cancer (UICC)
| TNM classification for testicular cancer | ||||
| pT – Primary Tumour1 | ||||
| pTX | Primary tumour cannot be assessed (see note1) | |||
| pT0 | No evidence of primary tumour (e.g., histological scar in testis) | |||
| pTis | Intratubular germ cell neoplasia (carcinoma in situ)+ | |||
| pT1 | Tumour limited to testis (including rete testis) and epididymis without vascular/lymphatic invasion and without invasion of the epididymis*# | |||
| pT2 | Tumour limited to testis with vascular/lymphatic invasion, or invading hilar soft tissue or the epididymis or tumour extending through tunica albuginea with involvement of visceral tunica vaginalis**# | |||
| pT3 | Tumour invades spermatic cord with or without vascular/lymphatic invasion** | |||
| pT4 | Tumour invades scrotum with or without vascular/lymphatic invasion | |||
| N – Regional Lymph Nodes – Clinical | ||||
| NX | Regional lymph nodes cannot be assessed | |||
| N0 | No regional lymph node metastasis | |||
| N1 | Metastasis with a lymph node mass 2 cm or less in greatest dimension or multiple lymph nodes, none more than 2 cm in greatest dimension | |||
| N2 | Metastasis with a lymph node mass more than 2 cm but not more than 5 cm in greatest dimension; or more than 5 nodes positive, none more than 5 cm; or evidence of extranodal extension of tumour | |||
| N3 | Metastasis with a lymph node mass more than 5 cm in greatest dimension | |||
| Pn – Regional Lymph Nodes – Pathological | ||||
| pNX | Regional lymph nodes cannot be assessed | |||
| pN0 | No regional lymph node metastasis | |||
| pN1 | Metastasis with a lymph node mass 2 cm or less in greatest dimension and 5 or fewerpositive nodes, none more than 2 cm in greatest dimension | |||
| pN2 | Metastasis with a lymph node mass more than 2 cm but not more than 5 cm in greatest dimension; or more than 5 nodes positive, none more than 5 cm; or evidence of extranodal extension of tumour | |||
| pN3 | Metastasis with a lymph node mass more than 5 cm in greatest dimension | |||
| M – Distant Metastasis | ||||
| MX | Distant metastasis cannot be assessed | |||
| M0 | No distant metastasis | |||
| M1 | Distant metastasis ** | |||
| M1a Non-regional lymph node(s) or lung metastasis | ||||
| M1b Distant metastasis other than non-regional lymph nodes and lung | ||||
| S – Serum Tumour Markers (Pre-chemotherapy) | ||||
| SX | Serum marker studies not available or not performed | |||
| S0 | Serum marker study levels within normal limits | |||
| LDH (U/l)< 1.5 x N and1.5-10 x N or> 10 x N or | hCG (mIU/mL)< 5,000 and5,000-50,000 or> 50,000 or | AFP (ng/mL)< 1,0001,000-10,000> 10,000 | ||
| S1S2S3 | ||||
European Association of Urology (n.d)
https://uroweb.org/guidelines/testicular-cancer/chapter/staging-amp-classification-systems
N indicates the upper limit of normal.
LDH = lactate dehydrogenase; hCG = human chorionic gonadotrophin; AFP = alpha-fetoprotein.
1 Except for pTis and pT4, where radical orchidectomy is not always necessary for classification purposes, the extent of the primary tumour is assessed in the radical orchidectomy specimen; see pT. In other circumstances, TX is used if no radical orchidectomy has been performed.+ The current “Carcinoma in situ” nomenclature is replaced by GCNIS.
* AJCC eighth edition subdivides T1 Pure Seminoma by T1a and T1b depending on size no greater than 3 cm or greater than 3 cm in greatest dimension.
** AJCC eighth edition considers hilar soft tissue invasion and epididymal invasion as pT2, while the discontinuous involvement of the spermatic cord is considered as pM1
# As updated in the UICC 8th Edition Errata.
Key Steps In The Diagnosis of Testicular Cancer
Step One
Previous Surgery
Example 1 of previous surgery: orchipexy due to cryptorchidism.
This procedure involves moving testicles from the abdomen or groin to the scrotum. To untangle or untwist the testicles from the spermatic cord.
Undescended Testicles and Orchiopexy – Video explanation
Example 2 of previous surgery: Inguinal hernia repair
Inguinal hernia is the swelling or lump caused by abdominal tissue pushing through weak spot in the top inner thigh groin. This is referred as the inguinal canal that can enter through abdominal wall near groin.
This can be resolved through a keyhole surgery or a cut in the inner thigh groin (National Health Service, 2025; Drugs.com, 2024). The open surgery involves cut in the inner thigh groin and push herniated tissue into position and repair opening with stitches or synthetic mesh to prevent future hernias.
In contrast, laproscopic surgery involve three incisions in the abdominal wall, inflate stomach with harmless gas, a tube-like instrument with small video camera called a laproscope can enter through incisions as well as surgical instruments. Using the monitor, the surgeon places herniated intestine into position and staple it (Drugs.com, 2024).
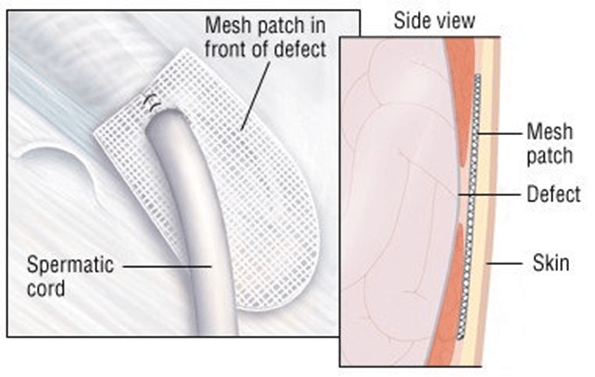
(Drugs.com, 2024)
Step Two
Step Three
Step Four
Trans-scrotal ultrasound
This is performed for suspected testicular cancer post-physical examination. This increases sensitivity to nearly 100%.
On the ultrasound, there are differences per type of testicular cancer.
Pathology: There is a hypoechoic, solid, vascularized intratesticular lesions (Gaddam, Bicer and Chesnut, 2023)
Normal testis: There is slightly low echogenicity in pre-puberty than adult testes. Mildly coarse.
Rete testis can be seen in 20% of patients where it appears hypechoic near mediastinum and become more noticeable if dilated.
The tunica albuginea/vaginalis has linear echogenic testicular mediastinum (Sharma, 2024).
Magnetic Resonance Imaging (MRI)
MRI is occasionally used for problem solving if the diagnosis is unclear on ultrasound.
Computed Tomography
Some researchers in the field consider CT rarely needed and should be avoided due to ionizing radiation. However, other researchers consider that cross-sectional imaging of the abdominopelvic region is needed for all germ cell tumours in the following situations:
To identify retroperitoneal lymph node disease arising from the primary testis cancer.
Patients with high levels of AFP, β-hCG and LDH should undergo CT of the chest, abdomen and pelvis for staging (Stephenson et al., 2019).
If normal levels, it is rare metastasis outside retroperitoneal lymph node.
CT scan of the brain in cases of choriocarcinoma and high levels of β-hCG as researchers shown tumour to go through hematogenous routes.
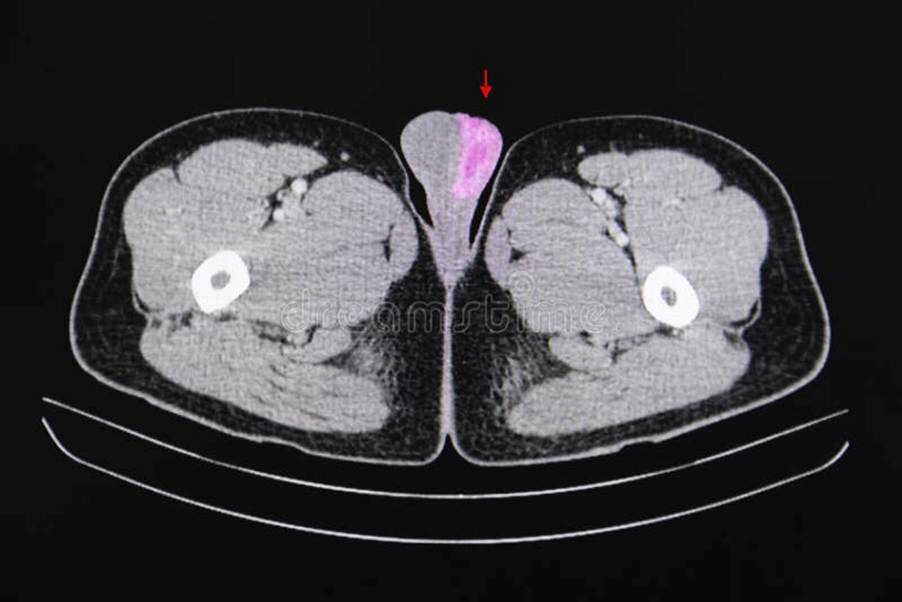
CT scan of the testicular region and surrounding tissue (Dreamtimes, 2025)
Radical inguinal orchiectomy
This is used for histopathological diagnosis for staging and therapy.
An 3 to 5cm incision is made along the Langer’s lines in the groin. The testicle, epididymis and spermatic cord and tumour mass are removed to the level of inguinal ring. If this does not work, it is done inferiorly to anterior scrotum.
Care must be taken following surgery such as avoiding heaving lift and high impact exercises. Supportive underwear to prevent swelling in the scrotum and hematoma (accumulation of blood in tissues that can cause swelling).
If the retroperitoneal lymph node have been removed/dissected, postoperative rehabilitation is commonly taken.


Video explanation on Orchidectomy
Transscrotal Biopsy
This procedure of taking a biopsy from outside the scrotum and into the testicle. It is done to determine the stage.
It is advised not to do so because there is a risk of draining of:
Lymph system of the testicles drawn into the abdomen.
Lymph system of scrotum drawn into lower legs (limbs)
In both scenarios, it can increase spread and influence management. There is an increase of local recurrence with this procedure (2.9%) more than orchiectomy (0.4%) (Capelouto et al., 1995).
References
Badia, R.R., Abe, D., Wong, D., Singla, N., Savelyeva, A., Chertack, N., Woldu, S.L., Lotan, Y., Mauck, R., Ouyang, D., Meng, X., Lewis, C.M., Majmudar, K., Jia, L., Kapur, P., Xu, L., A. Lindsay Frazier, Margulis, V., Strand, D.W. and Coleman, N. (2021). Real-World Application of Pre-Orchiectomy miR-371a-3p Test in Testicular Germ Cell Tumor Management. The Journal of Urology, 205(1), pp.137–144. doi:https://doi.org/10.1097/ju.0000000000001337.
Capelouto, C.C., Clark, P.U., Ransil, B.J. and Loughlin, K.R. (1995). Original Articles: Testis Cancer: A Review of Scrotal Violation in Testicular Cancer: Is Adjuvant Local Therapy Necessary? 153(3S), pp.981–985. doi:https://doi.org/10.1016/s0022-5347(01)67617-1.
Check 4 Cancer (2021) Have you got the balls to check yourself? Available at: https://www.check4cancer.com/advice-and-awareness/blog/1602-have-you-got-the-balls-to-check-yourself (Accessed: 4th July 2025)
Drugs.com (2024) Inguinal hernia Available at: https://www.drugs.com/health-guide/inguinal-hernia.html (Accessed: 4th July 2025)
European Association of Urology (n.d.) 4. Staging & Prognosis Available at: https://uroweb.org/guidelines/testicular-cancer/chapter/staging-amp-classification-systems (Accessed: 4th July 2025)
Gaddam, S.J., Bicer, F., Chesnut, G. (2023) Testicular Cancer. Available at: https://www.ncbi.nlm.nih.gov/books/NBK563159/ (Accessed: 3rd July 2025)
Gru, A.A., Williams, E.S. and Cao, D. (2017). Mixed Gonadal Germ Cell Tumor Composed of a Spermatocytic Tumor-Like Component and Germinoma Arising in Gonadoblastoma in a Phenotypic Woman With a 46, XX Peripheral Karyotype. American Journal of Surgical Pathology, 41(9), pp.1290–1297. doi:https://doi.org/10.1097/pas.0000000000000888.
Milose, J. Filson, C., Weizer, A., Hafez, K.S., Montgomery, J.S. (2011) Role of biochemical markers in testicular cancer: diagnosis, staging, and surveillance. Open Access Journal of Urology, 30, 4, pp. 1-8 doi:https://doi.org/10.2147/oaju.s15063.
National Health Service (2025) Inguinal hernia repair. Available at: https://www.nhs.uk/tests-and-treatments/inguinal-hernia-repair/ (Accessed: 4th July 2025)
Pedrazzoli, P., Rosti, G., Soresini, E., Ciani, S. and Secondino, S. (2021). Serum tumour markers in germ cell tumours: From diagnosis to cure. Critical Reviews in Oncology/Hematology, 159, p.103224. doi:https://doi.org/10.1016/j.critrevonc.2021.103224.
Sharma, R. (2024) Testicular and scrotal ultrasound. Available at: https://radiopaedia.org/articles/testicular-and-scrotal-ultrasound?lang=us (Accessed: 4th July 2025)
Stephenson, A., Eggener, S.E., Bass, E.B., Chelnick, D.M., Daneshmand, S., Feldman, D., Gilligan, T., Karam, J.A., Leibovich, B., Liauw, S.L., Masterson, T.A., Meeks, J.J., Pierorazio, P.M., Sharma, R. and Sheinfeld, J. (2019). Diagnosis and Treatment of Early Stage Testicular Cancer: AUA Guideline. Journal of Urology, 202(2), pp.272–281. doi:https://doi.org/10.1097/ju.0000000000000318.
Updated July 2025 Next Review April 2027



Leave a comment